Moving the Needle- A Quality Improvement Initiative to Improve Access for Autism Diagnostic Evaluations
April 23, 2020
|
The Waisman Center Autism and Developmental Disabilities Clinic is an interdisciplinary clinic that provides comprehensive diagnostic evaluations and ongoing medical care for infants, children and adolescents who have or are at risk for autism spectrum disorder or other significant neurodevelopmental disabilities. Our clinic team is composed of developmental behavioral pediatricians, audiologists, psychologists, speech language pathologists, occupational therapists, nurses and nurse practitioners, social workers, and medical assistants. Referrals to our clinic come from throughout the state of Wisconsin and northern Illinois. We receive over 900 referrals per year. Similar to other centers through the United States, our wait time for evaluation ranges from 7 months to over 15 months.

Picture: Lindsay McCary PhD, Madeline Barger LMFT, BCBA, Kathleen Kastner MD, Hayley Crain PsyD
We know that early identification of and intervention for individuals with autism spectrum disorder (ASD) is critical.1-3 Given the high volume of referrals, a delay in accessing initial evaluation services creates a barrier to early intervention, especially for young children who could potentially access intensive autism treatment services. The traditional diagnostic evaluation model at our center involves an initial half-day appointment (either with a developmental pediatrician or a psychologist) often followed by another 90-minute visit with the other provider on a different day as well as subsequent evaluations with other disciplines. This quality improvement initiative was designed to implement an abbreviated evaluation model, matched to the needs of the child, with the aim to shorten wait times for diagnostic evaluations for children under 3 years of age. We developed this project in coordination with clinic staff who are part of the University Center for Excellence in Developmental Disabilities (UCEDD) and a social work Leadership Education in Neurodevelopmental and Related Disabilities (LEND) trainee. This quality improvement project was inspired by the patients we serve with autism spectrum disorder, as we recognize the unique needs of different patients require a different approach to the diagnostic process.
Development of Modified Triage System
We collaborated with our LEND program, as a second year LEND trainee developed a pre-visit screening questionnaire with one of our family navigators. This questionnaire is completed with families on the phone at the time of referral to determine the appropriate evaluation type. The family navigators within our clinic have extensive knowledge on autism symptomology, which is an essential feature of our pilot project, as it allowed us to pre-screen children for diagnostic criteria.
Initial criteria for participation includes children under three years old, English speaking, and ASD concern noted by pediatrician. After the screening if ASD seemed likely based on our pre-visit screening tool and family was in agreement, an abbreviated visit was scheduled.
Table 1: Patient Demographics
|
Patient Characteristics |
|
|
Primary Insurance |
|
|
Private |
11 (44%) |
|
Medicaid |
14 (56%) |
|
Ethnicity/Race |
|
|
White/Caucasian |
15 (60%) |
|
Black/African-American |
3 (12%) |
|
Asian |
5 (20%) |
|
Hispanic |
2 (8%) |
|
Sex |
|
|
Male |
16 (64%) |
|
Female |
9 (36%) |
|
Age |
|
|
18-24 months |
7 (28%) |
|
25-36 months |
18 (72%) |
The alternative evaluation model included developmental cognitive testing with the Bayley Scales of Infant Development 4th Edition (Bayley-4), physical exam, Adaptive Behavior Assessment System - Third Edition (ABAS), developmental interview, and autism specific assessment using the Childhood Autism Rating Scale 2nd Edition (CARS-2). CARS-2 was selected due to its abbreviated length and current requirements in our state for the necessary components of an autism diagnostic evaluation in order to access treatment services. Total evaluation length was 2 hours with the option for families to meet with a family navigator afterwards to further discuss resources.
If the diagnostic impression was not clear after this shorter evaluation, then clinicians recommended returning for an Autism Diagnostic Observation Schedule 2nd Edition (ADOS-2) evaluation. This model allowed for two children to receive a full diagnostic evaluation per half day session. Our LEND social work trainee followed up with families post-evaluation to assess satisfaction.
Figure 1: Diagnostic Evaluation Process
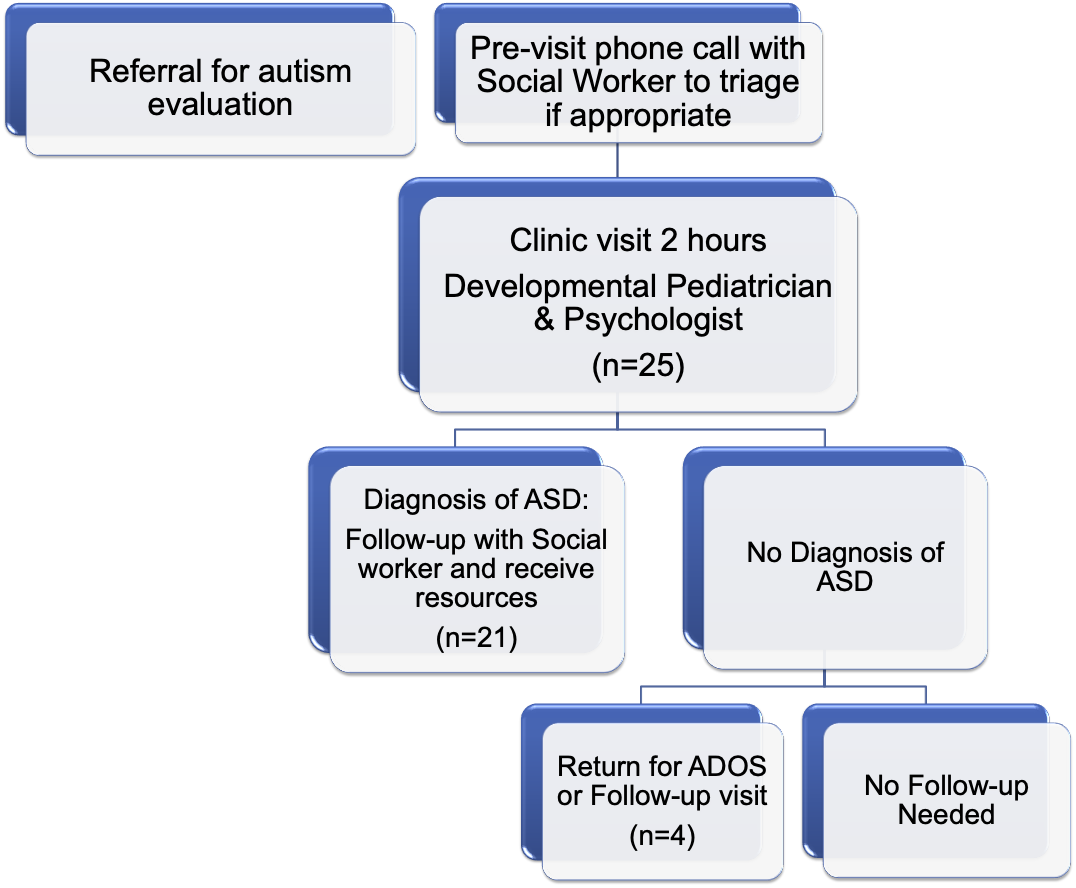
Figure 2: Intervention outcomes
|
|
Pre-intervention group |
Intervention group |
|
Time from referral to evaluation |
6.93 months |
4.25 months |
|
Total clinician time |
5.25 hours |
4.23 hours |
Graph 2: Family Satisfaction Data

Graph 2: Family satisfaction data collected at least 2 weeks following evaluation. Ratings range from 1 (poor or very dissatisfied) to 5 (excellent or very satisfied).
Traditional evaluations for ASD are one factor that can lead to increased wait times, but a multifaceted approach is likely necessary to fully address the problem. Novel strategies, such as alternative evaluation models, are one potential strategy to decrease wait times while maintaining high-quality, interdisciplinary care. Based on our pilot study, for patients with a high likelihood of an ASD diagnosis, this alternative evaluation model allows for shorter evaluation lengths without comprising family satisfaction or quality care. This model was appropriate for individuals under three, with English as their primary language.
Next steps/Future Directions
Our next steps include: 1) expand the alternative evaluation model to include non-English speaking families; 2) explore characteristics of children who were recommended to return for further evaluation to refine our criteria regarding which patients are appropriate for this alternative evaluation; 3) explore options for other potential evaluation tools to be used in lieu of, or in conjunction with, the CARS-2; and 4) explore options to adapt this process for patients over the age of three.
Resources:
- Gordon-Lipkin E. et al. Pediatr. Clin. North Am. 63, 851-859 (2016)
- Austin J. et al. Pediatrics 137 Suppl 2, 149-157 (2016)
- Gerdts J. et al. J. Dev. Behav. Pediatr. 39, 271-281 (2018)







