Building an Autism Friendly Hospital: How we started, what we have accomplished, and where we go from here
December 18, 2019
Hospital visits can be particularly challenging for patients with Autism Spectrum Disorder (ASD) if their unique communication, sensory, and safety/behavioral needs are unaddressed1,2 (Figure 1). This is especially concerning as individuals of all ages with ASD have been found to have higher rates of various medical conditions, and are thus subject to higher healthcare utilization and costs3-6.

Figure 1 - Visual representation of sensory and communication barriers for patients with ASD
Children with ASD experience more inpatient and outpatient visits than their neurotypical peers, and are often prescribed more medications. Further, annual healthcare costs for children with ASD are approximately seven times higher than their neurotypical peers4. In spite of the higher levels of reported utilization, however, caregivers of children with ASD were significantly more likely to report difficulty using services, lack of shared decision making and care coordination, and adverse family impact as compared to caregivers of children with other developmental disabilities, mental health conditions, or both7. There is a troubling disconnect between the heightened frequency of these patients' visits and lower quality of the resulting encounter.
To improve the hospital experience for patients with ASD and their families, the Autism Program at Boston Medical Center (BMC) launched the Autism Friendly Initiative in January 2017. The initiative began with the formation of a multidisciplinary steering committee involving clinicians and staff from various departments across the hospital (e.g., Nursing, Dental, Facilities, and Security) as well as parents of individuals with ASD. The steering committee continues to meet routinely to discuss the status of efforts launched by the initiative. One of these early efforts launched by the Autism Friendly Initiative was a comprehensive needs assessment consisting of several sub-projects that examined the healthcare utilization needs and patterns of patients with ASD at BMC (Table 1). Findings from some of these projects have been presented nationally.
|
Project Name |
Description |
Key Findings |
|
Hospital-wide staff survey |
Online survey to all hospital staff (n=110) about caring for patients with ASD. |
· 50% reported being uncomfortable caring for patients with ASD · Many reported wanting more resources and training
|
|
Parent focus group |
Focus group on hospital experiences of parents (1 male, 8 females) who have children ages 3-28 with ASD (n=9). Four themes were extracted from parents' responses. |
· Lack of provider knowledge · Waiting room environment or sensory overload · Provider inflexibility · Parents as experts of their children's needs
|
|
Literature review |
Building ongoing repository of journal articles regarding the healthcare needs and experiences of individuals with ASD |
· Patients with ASD have higher healthcare needs, utilization, and costs. · Despite higher use, patients with ASD and families reported lower care satisfaction. · Limited information on ASD adult population.
|
|
Ethnographic study |
Followed 16 patients (12 male, 4 female) ages 3-17 during an outpatient visit between January and March 2018.
|
· Identified barriers to patient care: patient behavior, hospital environment, and communication.
|
|
Patient data analysis |
Retrieved data from BMC clinical data warehouse for patients with ICD-9 and ICD-10 codes who were seen in 2017. |
· 1,787 unique pediatric (≤22 years old) patients generated 8,000 encounters. 304 unique adult (≥23 years old) patients generated 1,953 encounters. · The ED was one of the most visited departments for all patients (#4 for pediatric and #2 for adult patients). · 1 in 4 pediatric ED encounter was due to behavioral/situational crisis. |
Table 1 - List of needs assessment projects implemented at the start of the Autism Friendly Initiative.
Informed by engaged stakeholders and findings from the needs assessment projects, the Autism Friendly Initiative team developed and launched interventions that fall within four categories, namely (1) communication, (2) knowledge, and (3) sensory accommodations.
Communication: Individualized care plans, visit preparation, Healthcare Social Stories application, and case coordination
Individualized Care Plans
Each individual with ASD has unique sets of needs and challenges, which can weigh heavily on the ultimate success of a clinical visit. To help inform clinicians on how they can accommodate different and unique patients during their visit, the Autism Friendly Initiative developed and implemented an Autism Support Checklist (ASC) (Figure 2), a questionnaire that collects information about a patient's communication style, triggers, safety concerns, and de-escalation strategies. It is administered by phone, and information gathered through the ASC is summarized and entered into the patient's Electronic Medical Record (EMR) for their clinicians to access (Figure 3). The ASC is posted prominently within the EMR, and is available to any clinician or staff member, wherever a patient is seen, regardless of any prior relationship. Currently, the ASC is available in English, Spanish, Portuguese, Arabic, Traditional Mandarin, and Simplified Mandarin.
By December 2019, 430 ASCs have been completed, primarily for patients who were seen within the Developmental and Behavioral Pediatrics division at BMC Moreover, we have also completed a research study investigating two implementation strategies for the ASC. We found that the ASC is generally well-received by clinicians and that an active, in-person training may improve clinician engagement (i.e., the likelihood of the clinician to read the ASC). We presented these findings at the 12th Annual Conference on the Science of Dissemination and Implementation in Health in Washington, DC.
Moving forward, the initiative is working with stakeholders across the hospital to update the EMR system to allow staff to capture accessibility-related needs, including an ASD diagnosis, at the point of patient registration. Furthermore, the Autism Friendly Initiative team is working to expand the reach of the ASC to other sections of the hospital, with plans to launch ASC collection for Pediatric Neurology and Pediatric Primary Care in early 2020. The ultimate goal is to assure that any patient with ASD that comes to BMC has an ASC in their medical record.

Figure 2 - A sectional view of the Autism Support Checklist (ASC).
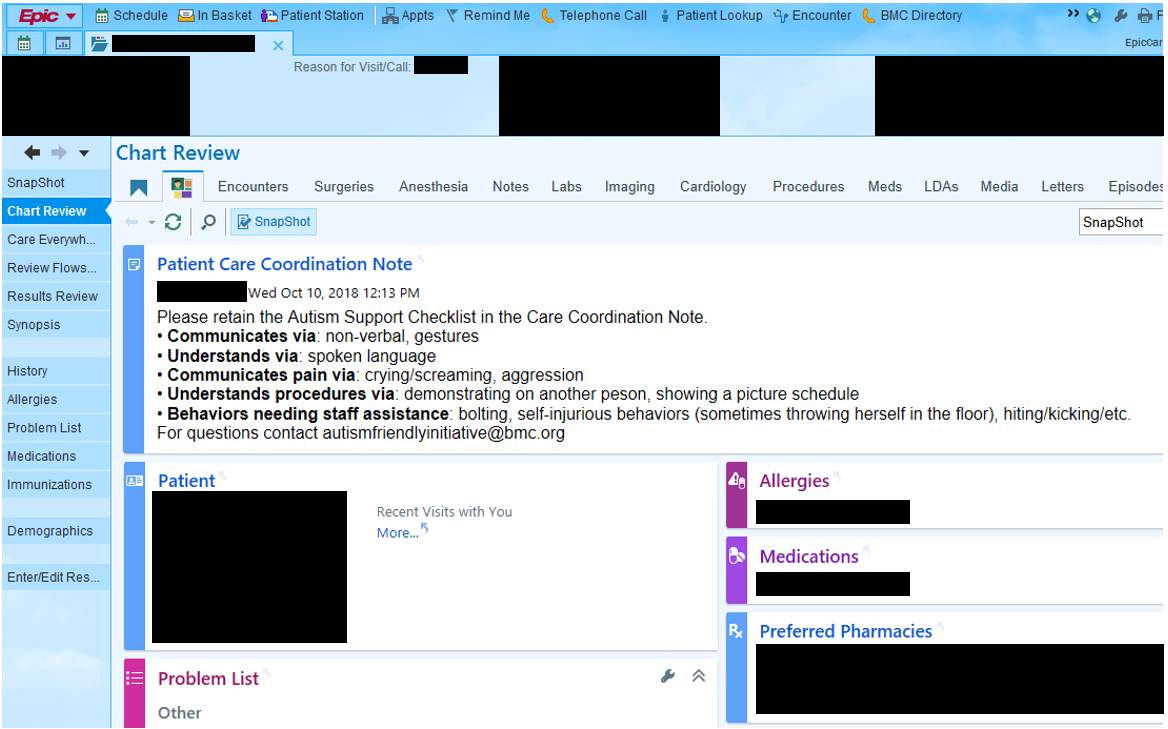
Figure 3 - A clinician's view of the Autism Support Checklist (ASC) in the patient's electronic medical record.
Visit Preparation
Another common feature of the ASD diagnosis is a preference for structured routine, and consequential distress if such routine is disrupted8. This is why steps to preemptively prepare patients with ASD for a hospital visit can be crucial to ensuring that the visit is completed successfully. The Initiative has launched two interventions to approach this challenge, (1) Healthcare Social Stories Website-based Application and (2) Individualized Case Coordination.
Healthcare Social Stories Application
The Healthcare Social Stories Application is a website-based tool using "Social Stories" to help patients with ASD spatially navigate their BMC visits by breaking down steps using simple narratives, pictures, and built-in reinforcements (e.g., gold star) (Figure 4). Social Stories is a widely used tool to teach individuals with ASD about complex social situations (e.g., going to a restaurant, playing with friends) by breaking them down into smaller, easy-to-follow steps with visual and written prompts9. The Healthcare Social Stories Application is customizable based on patient gender, transportation mode to BMC, clinic location, and type of visit (e.g., routine check-up, blood-draw, x-ray, etc.). Moving forward, the initiative is working to convert the website-based application into a free downloadable mobile application. Moreover, the initiative is exploring enhancements such as building a library for users to create and save their own personalized Social Stories.
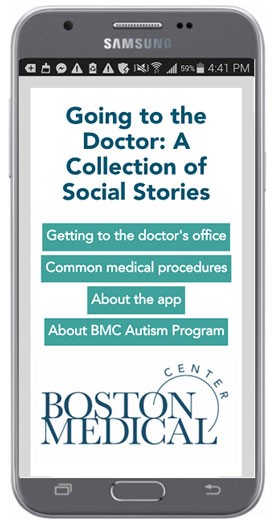
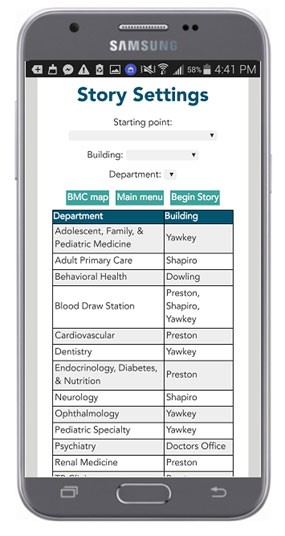

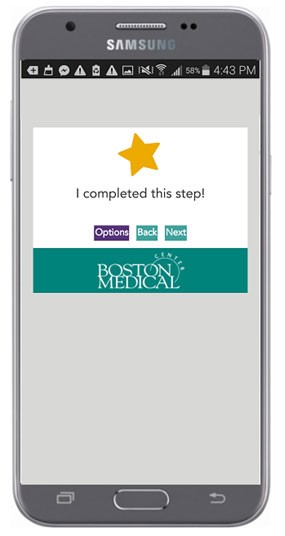
Figure 4 - Visual representation of the Healthcare Social Stories Application.
Case Coordination
In addition to the Healthcare Social Stories Application, the initiative is expanding the role of the Autism Program's Autism Resource Specialists (ARS) to support patients with ASD, anywhere they are seen within the hospital. While historically these staff have worked squarely within Developmental and Behavioral Pediatrics, the expanded role allows broader coordination within departments and care coordination of patients and families prior and throughout the visit, anywhere in the hospital. To date, Autism Resource Specialists have collaborated with such departments as Ophthalmology, Psychiatry, Primary Care, and the pediatric Dental clinic to provide this individualized support.
Knowledge: Autism 101 trainings, Doctor's Day, training videos
There are three types of training modalities that the Autism Friendly Initiative team has implemented to address the reported lack of comfort, knowledge, and familiarity on the part of clinicians working with patients who have ASD. These modalities include (1) Autism 101, (2) Doctor's Day, and (3) Training Videos.
Autism 101 Trainings
The Initiative regularly delivers 90-minute "Autism 101" trainings to (1) third year Boston University School of Medicine (BUSM) students (2) BMC's Department of Public Safety for all of their new hires, (3) Interpreter Services, (4) Genetics Counseling Students, and (5) BU Dental School Students and residents. The Autism 101 trainings consist of two components, namely (1) lecture and (2) parent panel, providing unique rich insight into the family experience, and what clinicians and staff need to know when caring for patients with ASD and their families (Figure 5).

Figure 5 - Parent panel consisting of three parents of children with ASD at an Autism 101 training.
In addition to regularly conducting the Autism 101 trainings, we are also concurrently studying their effectiveness in improving participants' self-reported knowledge and comfort with the diagnosis, as well as gathering qualitative feedback. Specifically, we administer one survey before and one survey after the training to third year medical students who participate in the Autism 101 trainings, for a total of two surveys. We compare the changes in four survey items before and after the training, namely: (1) familiarity with ASD, (2) familiar with techniques to accommodate patients with ASD, (3) comfort in examining patients with ASD, and (4) comfort in communicating with patients with ASD (Figure 7). To date, we have collected surveys from over 200 medical students and statistical significance in increases before and after training across all four aforementioned survey items (Table 2).
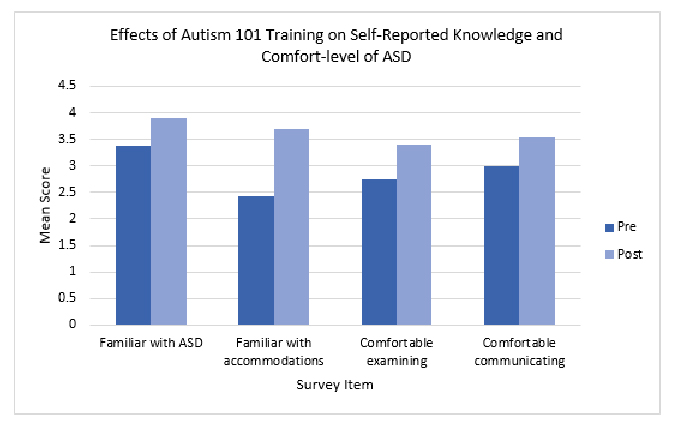
Figure 6 - Bar graph representing the changes in familiarity with ASD, familiarity with techniques to accommodate patients with ASD, comfort in examining a patient with ASD, and comfort in communicating with a patient with ASD.
|
Survey Item |
Pre-training Mean (N = 243) |
Post- training Mean (N = 241) |
t |
df |
P-value |
|
How familiar are you with autism spectrum disorders (ASD)?
|
3.38 |
3.91 |
-9.26 |
464.6 |
.000
|
|
How familiar are you with techniques for accommodating patients with ASD?
|
2.44 |
3.69 |
-17.81 |
451.5 |
.000
|
|
How comfortable are you examining a patient with ASD?
|
2.74 |
3.41 |
-8.22 |
481 |
.000
|
|
How comfortable are you communicating with a patient with ASD? |
2.99 |
3.54 |
-7.22 |
481 |
.000
|
Table 2 - Results of independent samples t-test comparing the means of participant responses before and after the Autism 101 training. Significance is considered at p < 0.05.
In addition, participants also rated the trainings positively, particularly with the inclusion of the families' perspectives. For example:
"I've previously worked in the autism community and considered becoming a developmental specialist - this [training] really reinvigorated that desire. I will definitely use a lot of the tools and strategies discussed today, and invest in an ASD toolbox for my future office!"
"Having the parent panel was excellent and provided great insight to these patients' stories"
Doctor's Day
Doctor's Day is an annual event that is implemented in collaboration with Boston Public Schools, and specifically the Joseph Lee Elementary School (Figure 6). During the event, BUSM students volunteer to help children with ASD complete simulated medical check-ups (e.g., height and weight, blood pressure measurement, look in ear). Each year, Doctor's Day serves approximately 200 students with ASD aged 3-14. This event provides (1) medical students with experiential training in working with patients with ASD and (2) children with ASD the exposure of common medical procedures in a safe and fun environment.

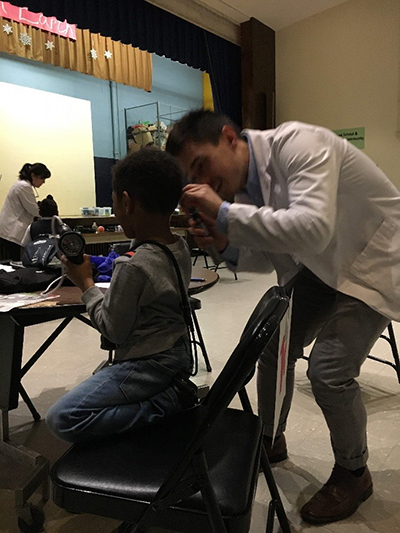
Figure 7 - A medical student and an elementary student with ASD practicing a simulated "check-up".
Training Videos
To improve the accessibility and broaden the reach of our trainings, we have developed four professionally produced 5-min training videos for clinicians and staff around the following topics: (1) what is autism, (2) sensory accommodations, (3) communication accommodations, and (4) managing behavior and assuring safety. The videos include patient roleplay and family interviews, as well as perspectives from clinicians. As part of our future directions, we hope to include these training videos in annual compliance for BMC employees and standard onboarding orientation protocols.
Sensory Accommodations: Sensory toolbox
Lastly, to address the sensory sensitives and aversions that patients with ASD may experience, the Autism Friendly Initiative developed and distributed Sensory Toolboxes in collaboration with BMC's Child Life Department (Figure 7). The Sensory Toolbox contains several different sensory items to calm, distract, and redirect patients with ASD during a visit. Examples of items include: (1) sunglasses, (2) noise-cancelling headphones, (3) weighted lap pad, and (4) visual timer. To date, over 20 toolboxes have been distributed to departments across BMC and our team collaborates with toolbox champions in each department to implement and maintain the toolboxes. Furthermore, the team also regularly conducts trainings every time a toolbox is distributed to a new department. To measure usage and user satisfaction, we consistently collect data under supervision from our Quality Improvement Board.

Figure 8 - the Sensory Toolbox available to patients with ASD with sensory aversions/sensitivities.
The goal of each of the aforementioned interventions is to lead to better hospital experiences and ultimately better healthcare outcomes for patients with ASD. In isolation, these interventions would likely be less effective than they are as part of a greater whole. For example, knowing about a patient's need for sunglasses cannot help if the clinician does not have sunglasses to offer. One provider dimming their exam room lights will not be very effective if the patient has just spent an hour in a jarringly bright waiting room. As we continue to implement existing interventions and explore opportunities to further support patients with ASD and staff at every level of the institution, we are also rigorously studying and disseminating our work. Some examples of conferences in which we have presented our Autism Friendly work include: (1) Pediatric Academic Society (PAS); (2) Annual Meeting of the Massachusetts Early Intervention Consortium Conference; and (3) International Society for Autism Research (INSAR) Annual Meeting. Public understanding and involvement at a systemic level are crucial if the goal is to achieve widespread implementation of Autism Friendly practices. This kind of holistic approach can be adapted or tailored to a given healthcare system or department's unique needs, but the key features of an Autism Friendly system are conserved, namely by (1) gathering information from relevant stakeholders, (2) developing evidence-informed interventions, and (3) disseminating these strategies to improve the hospital experience and health outcomes of patients with ASD.
References
- Nicolaidis C, Raymaker DM, Ashkenazy E, et al. "Respect the way I need to communicate with you": Healthcare experiences of adults on the autism spectrum. Autism. 2015;19(7):824-831. doi:10.1177/1362361315576221
- Muskat B, Burnham Riosa P, Nicholas DB, Roberts W, Stoddart KP, Zwaigenbaum L. Autism comes to the hospital: The experiences of patients with autism spectrum disorder, their parents and health-care providers at two Canadian paediatric hospitals. Autism. 2015;19(4):482-490. doi:10.1177/1362361314531341
- Cummings JR, Lynch FL, Rust KC, et al. Health services utilization among children with and without autism spectrum disorders. J Autism Dev Disord. 2016;46(3):910-920. doi:10.1007/s10803-015-2634-z
- Liptak GS, Stuart T, Auinger P. Health care utilization and expenditures for children with autism: Data from U.S. national samples. J Autism Dev Disord. 2006;36(7):871-879. doi:10.1007/s10803-006-0119-9
- Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization utilization and costs of children with and without autism spectrum disorder in a large group-model health plan. Pediatrics. 2006;118(4):1203-1211. doi:10.1542/peds.2006-0127
- Croen LA, Zerbo O, Qian Y, et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814-823. doi:10.1177/1362361315577517
- Vohra R, Madhavan S, Sambamoorthi U, St Peter C. Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism. 2014;18(7):815-826. doi:10.1177/1362361313512902
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Gray CA, Garand JD. Social stories: Improving responses of students with autism with accurate social information. Focus Autistic Behav. 1993;8(1):1-10. doi:10.1177/108835769300800101







